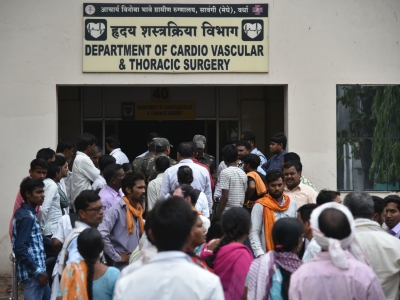
Nagpur, Dec 21 (IANS) The Comptroller and Auditor General of India (CAG) in its report has made scathing observations on Maharashtra’s public health infrastructure, saying that it was overburdened due to shortage of health care institutions, as a result of which they catered to population in excess of the norms laid down in the Indian Public Health Standards.
It also highlighted the shortage of manpower at the entry level.
The CAG report on public health infrastructure and management of health services in Maharashtra was presented in the state Assembly by Deputy Chief Minister Ajit Pawar on the last day of the Winter Session on Saturday.
“There was wide disparity in the population catered to by the Sub-Centres, Primary Health Centres and Rural Hospitals, indicating flaws in the plans to establish health care institutions. Nearly 70 per cent of the work of constructing new health care institutions and 90 per cent of the work of upgradation of health care institutions as per the master plan (January 2013 and June 2014) was not completed as of September 2022. Super Specialty Hospital (Phase II), Amravati constructed at the cost of Rs 31.91 crore in June 2015 remained unutilised for more than three years.
“Further, 433 works included in the master plan could not be started due to non-availability of land. The Government may ensure that a comprehensive plan to identify the gaps in infrastructure is prepared considering the projected population and implemented in a time-bound manner so that adequate health care institutions are available as per the Indian Public Health Standards. The Government may also ensure that land is identified for completion of medical infrastructure,” reads the report.
Commenting on the inadequate manpower, the CAG said the shortage of doctors, nurses and paramedical staff was 22 per cent, 35 per cent and 29 per cent respectively in primary and secondary health care under the Public Health Department.
In respect of women hospitals under the Public Health Department the shortage of doctors, nurses and paramedical staff was 23 per cent, 19 per cent and 16 per cent respectively.
There was also a shortage of 42 per cent in the cadre of the specialist doctors under the Public Health Department.
The shortage of doctors, nurses and paramedics under the Medical Education and Drugs Department was 37 per cent, 35 per cent and 44 per cent respectively.
The overall shortage in the cadre of doctors, nurses and paramedics in the state under the Public Health Department and Medical Education and Drugs Department was 27 per cent, 35 per cent and 31 per cent respectively.
The audit also noticed regional disparity in the shortage of manpower.
Similarly, the vacancies in the Trauma Care Centres under the Public Health Department and Medical Education and Drugs Department were 23 per cent and 44 per cent respectively.
The vacancies in the cadre of doctors, nurses and paramedical staff in AYUSH colleges and hospitals under the Medical Education and Drugs Department was 21 per cent, 57 per cent and 55 per cent respectively.
The sanctioned strength of doctors was less than the requirement as per Indian Public Health Standards, 2012 by 17 per cent under the Public Health Department.
“The Government may fill up the vacancies in the health sector in a time-bound manner to ensure optimal and qualitative delivery of healthcare services to the public.
“The Government may also increase the sanctioned strength of doctors under the Public Health Department as recommended in Indian Public Health Standards,” suggests the CAG.
According to CAG, Out-Patient Department services in hospitals were inadequate with 93 per cent of Rural Hospitals having only one registration counter as against two required as per Indian Public Health Standards in the seven selected districts.
The audit also noticed long waiting time for registration, and 26 per cent of doctors attending more than double the minimum number of patients as per Indian Public Health Standards.
Several specialist Out-Patient Department services such as general medicines, general surgery, dental services were not available in many of the district hospitals, women hospitals and hospitals attached to medical colleges.
“The government may ensure that specialist services such as general medicines, general surgeries, dental services are provided in all the health care institutions as per Indian Public Health Standards. The audit also noticed non-availability of radiology and imaging services. Government may ensure that essential radiology services such as X-ray, Ultrasonography and Mammography are made available in health care institutions as per Indian Public Health Standards” reads the report.
Patient-centric diet was not provided in 33 test-checked Sub-District and Rural Hospitals. Diet committees were not formed in seven (nine per cent) out of 78 test-checked health care institutions providing dietary services.
“Testing of food supplied by contractors was not done from the Public Health Laboratory by 16 test-checked health care institutions under the Public Health Department.
“The government may ensure that the nutritional requirements of patients are addressed by delivery of patient-centric diets,” reads the report.
Amid recent cases of fire in various hospitals, the CAG has suggested that the government may ensure that health care institutions comply with fire, electric and structural audit requirements in a time-bound manner.
“Failure to obtain No Objection Certificate from the Fire Department by 36 test-checked health care institutions, non-compliance to fire electric safety recommendations by all the test-checked health care institutions in eight selected districts and failure to take action on structural audit recommendations by eight test-checked health care institutions exposed the life of patients and staff and property to risk of fire” reads the report.
According to the CAG, the non-adoption of Clinical Establishment Act, 2010 in private nursing homes/health care facilities increased the risk of clinical establishments running without registration and deficiencies in providing proper health care by them.
“The Government may explore the possibility of adopting the Clinical Establishment Act, 2010 so that all the clinical establishments in the state are registered and are adequately monitored to ensure that minimum standards of facilities and services are provided to the public. The government may also ensure that the updated database of medical facilities is maintained,” reads the report.
(Sanjay Jog can be contacted on sanjay.j@ians.in)
–IANS
sj/rad
